Your coronavirus blood clot questions, answered
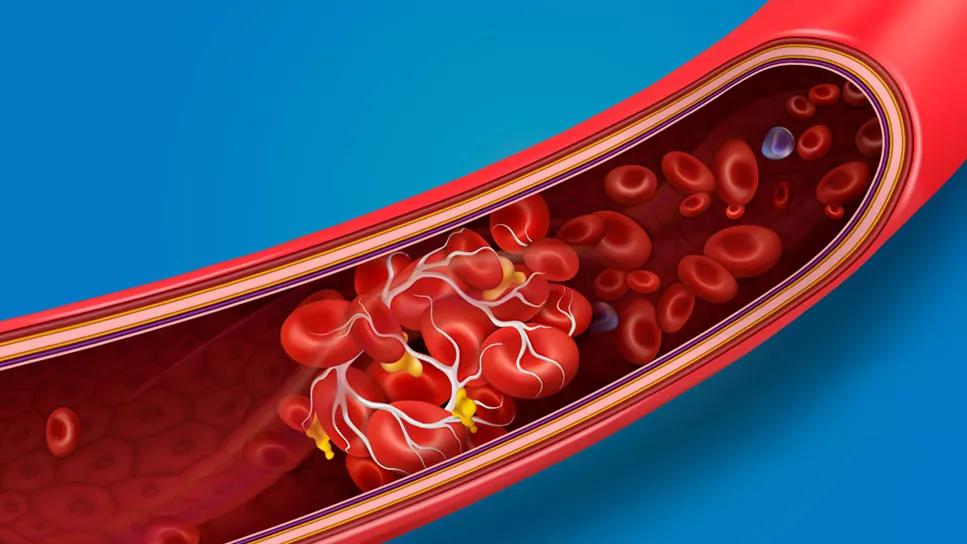
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9b2dae44-f4ab-409e-bdda-a63bc4f966bf/bloodClots-1172667442-770x533-1_jpg)
blood clot formation
Experts are still learning exactly how COVID-19 affects the body. One worrisome symptom that has emerged is blood clots.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We’re seeing a higher rate of blood clots in patients hospitalized with COVID-19,” says pulmonologist Wayne Tsuang, MD. “But it’s not clear yet how common clots are in people with mild symptoms who are at home.”
Blood clots are associated with serious complications, such as stroke. Scientists are scrambling to learn more about why the clots are occurring in coronavirus patients and who is most vulnerable. Here’s what we know so far.
A blood clot is a clump of blood. When blood clots, it changes from a liquid state to a thicker, gel-like state.
Clotting is your body’s natural way to stop bleeding. But when clots break free and travel through the bloodstream, they can block blood flow to essential organs such as the lungs (causing a pulmonary embolism) or brain (causing a stroke). “If the clots block a blood vessel, you can lose the blood supply to that organ,” Dr. Tsuang explains.
It’s not yet clear how or why COVID-19 is causing blood clots to form, Dr. Tsuang says. But there does seem to be a connection. One study in Amsterdam found that nearly one-third of people hospitalized with severe cases of COVID-19 had complications from blood clots.
Clots are most likely to arise in the blood vessels of the legs. People in the hospital are at higher risk, Dr. Tsuang explains.
Advertisement
“When you’re in the hospital, you’re not up and moving around, so blood moves more slowly through the legs. That makes clots more likely to form.”
“Doctors use a checklist to estimate the risk that a hospitalized patient has for developing blood clots,” Dr. Tsuang says. “Depending on the risk, there are therapies we can use to prevent clots from forming.”
Blood-thinning medications lower the risk for clots. Yet they also increase the risk of bleeding, so they aren’t always an option for high-risk patients.
Another way to prevent clots is to use special “boots” that wrap tightly around the legs. “The boots inflate with air to massage the legs and push the blood through, lowering the risk that a patient will develop blood clots,” Dr. Tsuang explains.
There are reports that clots are forming in people with COVID-19 who are at home and mobile — not just those lying flat in a hospital bed. But it’s not clear yet how common they are.
“When people are in the hospital, we’re more likely to do tests to look for clots. So we know more about this symptom in people with severe cases,” Dr. Tsuang explains. “In less ill patients who are recovering at home, we just don’t know yet.”
If you have other conditions that put you at risk for clots, your doctor may consider using a blood thinner to reduce your risk, Dr. Tsuang says. But there can be serious risks from increased bleeding, so don’t start any blood-thinning medications without consulting your doctor first.
The best thing you can do to reduce the risk, he adds, is to stay mobile. “Move around as much as you can. If you’re resting in bed, try to stretch your legs to keep blood circulating,” he says.
Some patients with the coronavirus have developed a symptom called “COVID toes” — red, swollen toes that might be due to small clots in the blood vessels of the feet. But it’s not clear how common COVID toes are.
In the legs, swelling is the most common sign of a blood clot, Dr. Tsuang says. “If you have significant swelling in one leg, call your doctor right away.”
There’s no reason to panic about clots, but it’s important to understand the risk, Dr. Tsuang says. If you’re being treated for COVID-19, start a conversation about blood clots with your medical providers.
“Ask your doctor about the best strategy,” he says. “The medical community is working toward finding the optimal strategy to prevent clots.”
Advertisement

Delivered every Tuesday!
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more
It's a letter about the news!

Every two weeks once
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
Bleeding is a risk and warrants taking care, but the reward of this lifesaving medication is great
Most recommended precautions center around minimizing bruising or swelling
Even one drink can have an impact on your cognitive function leading to slurred speech, blurred vision and impaired memory
Understand who may (and may not) benefit
Lorem ipsum dolor sit amet. Et odio Quis vel ipsam omnis eum alias deleniti et placeat impedit non voluptas galisum hic autem enim et cupiditate aliquid. Est beatae quidem non facilis autem ut commodi nisi aut tempore rerum et dolores voluptatem cum enim optio id sapiente quasi. Ad laboriosam officiis 33 cupiditate sequi ea voluptatum consectetur qui necessitatibus voluptate et quasi doloremque et facere explicabo quo explicabo officia
Seeking help through therapy can be an important step in improving your quality of life when you have UC
Type 2 diabetes isn’t inevitable with these dietary changes
Applying a hot or cold compress can help with pain
Pump up your iron intake with foods like tuna, tofu and turkey