Understanding food-drug interactions

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/72bfca64-aba9-4382-9ab2-02644cd858ae/eatGrapefruit-78567831-770x553_jpg)
woman eating grapefruit in bed
You’ve probably never thought about it, but your medications require a number of chemical and biological processes in your body to produce their intended benefit. And a number of factors — like what you’re eating and drinking, and when — can interfere, creating undesired (and potentially serious) effects.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Although some food-drug interactions are relatively mild, others can be severe.
“A lot of people think about drug-drug interactions, but they forget about food-drug interactions,” says Director of Pharmacy Mandy Leonard, PharmD, BCPS. “So it’s good to be educated about food-drug interactions as well.”
Grapefruit interactions:
One of the more well-known food-drug interactions involves grapefruit and grapefruit juice and certain cholesterol-lowering statin medications — namely, atorvastatin (Lipitor®), lovastatin (Mevacor®), pitavastatin (Livalo®) and simvastatin (Zocor®). Some compounds in grapefruit and grapefruit juice can block the action of an enzyme that metabolizes these drugs in your intestines. Consuming large quantities of grapefruit products while taking these statins can lead to greater concentrations of the medication in your bloodstream, increasing your risk of side effects.
Grapefruit and its juice may also interact with a number of other medications. These include certain calcium channel blockers (a class of blood pressure drugs), antibiotics, blood-thinning medications, erectile dysfunction (ED) drugs, and immunosuppressants, like cyclosporine.
With some medications, you can still enjoy limited amounts of grapefruit, Dr. Leonard says, while with others it’s best to eliminate it from your diet.
“We tell our transplant patients not to consume grapefruit at all if they’re on cyclosporine,” she advises. “I would even say that of the statins — I would just avoid it. Everybody’s metabolism is a little different. If someone forgets and has a glass of grapefruit juice, they’ll probably be fine, but they should keep from consuming it in their diet consistently.”
Advertisement
Vitamin K interactions:
Use of another widely prescribed medication, the anticoagulant drug warfarin (Coumadin®), requires careful and consistent intake of foods rich in vitamin K. These include green leafy vegetables, broccoli, cauliflower and canola oil. Changes in how much vitamin K you’re getting can affect warfarin’s activity.
Other nutrient or substance interactions:
Not only can foods affect the action of your medication. But some drugs can trigger potentially dangerous increases in certain nutrients or substances you get from food. For instance, some drugs interfere with caffeine metabolism. This causes you to have higher blood levels of caffeine, heightening its stimulating effects.
Certain blood pressure-lowering drugs — including angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs) and potassium-sparing diuretics — can lead to high potassium levels (hyperkalemia). This can trigger dangerous cardiac arrhythmias.
If you take these medications, your doctor will check your potassium levels periodically and may instruct you to avoid getting excess potassium from foods like bananas, orange juice and salt substitutes made with potassium. On the flip side, some diuretics — like hydrochlorothiazide, chlorthalidone, metolazone (Zaroxolyn®) and furosemide (Lasix®) — can cause potassium depletion. So you may be advised to consume more potassium in your diet.
Importantly, if you drink alcohol, be sure to ask your doctor if you can safely imbibe while taking a medication. Among its many potential interactions, alcohol can heighten the sedating effects of certain medications, interfere with some diabetes drugs and increase the risk of low blood sugar (hypoglycemia), and exacerbate the stomach-irritating effects of nonsteroidal anti-inflammatory drugs, such as aspirin, ibuprofen (Advil®, Motrin®) and naproxen (Aleve®).
“You can always ask your pharmacist to go over these interactions with you,” Dr. Leonard recommends. “With some of these foods, it’s not like you have to avoid them altogether, but you have to be careful about consuming them in moderation.”
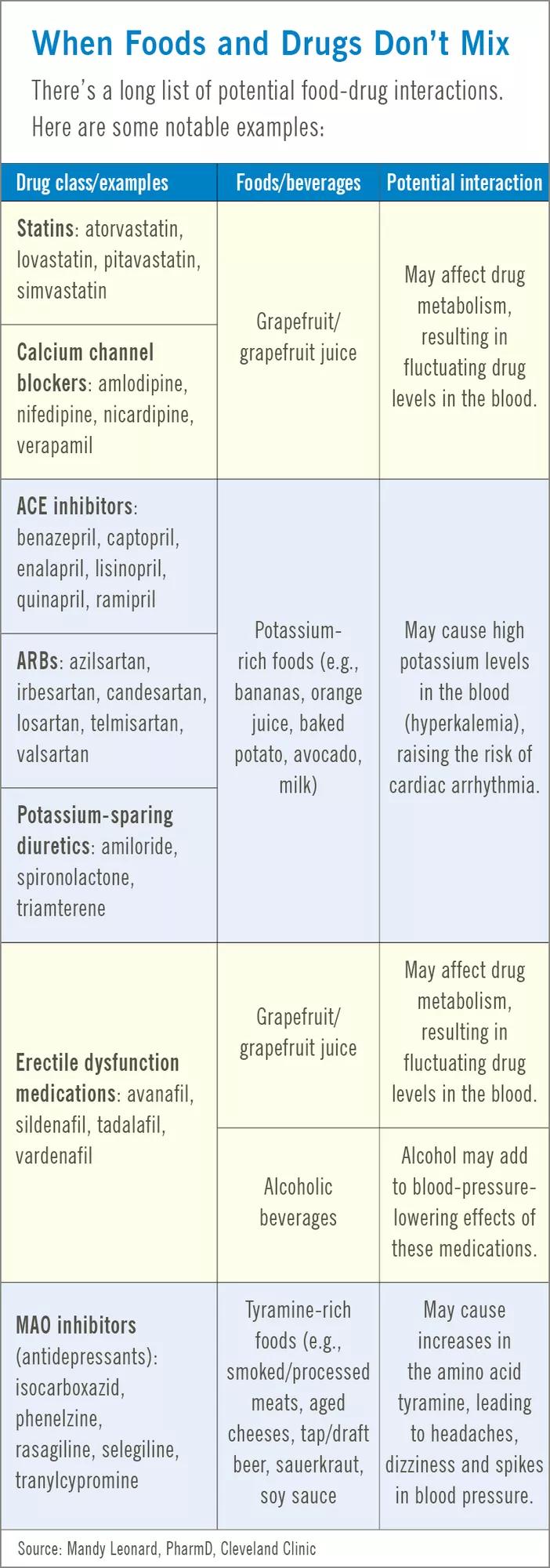
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a3299358-5982-4e8d-8907-a09a2030b17b/table-HEpost-foodDrugsDontMix_jpg)
How your medications work also can depend on when you take them vs. your mealtimes. Some can be taken with or without food.
Some, such as certain ACE inhibitors, bisphosphonate drugs (used to treat osteoporosis) and some heartburn medications, need to be taken on an empty stomach — or at least 30 minutes to a few hours before eating. In other instances, your doctor and pharmacist will advise you to take a medication with food to reduce stomach irritation and to improve the drug’s absorption and effectiveness.
Advertisement
Knowing when to eat and which foods you should or shouldn’t consume with food can be difficult, especially if you take multiple medications that have varying food requirements. So, talk with your pharmacist and use a pill organizer to help you structure the timing if your medications.
“It can be beneficial to have a plan laid out,” Dr. Leonard says. “Let’s say you’re on several different medications. Can you take all of them at breakfast? Should your take one at breakfast, one at lunch and one at dinner? It can become very confusing for patients. A pharmacist can really help you figure out not only which foods to avoid, but also when around meals a medication should be taken.”
The best way to prevent a food-drug interaction is to learn about the medications you take and heed the warnings on the drug label and the informational materials that accompany your prescription, Dr. Leonard says.
“You should read the prescription bottle and look at all the labels, and read the pamphlet that gets shoved in the bag with the bottle that some people don’t read,” she advises.
“Even more important is that if you have a relationship with your pharmacist, they can explain the information relatively quickly, and then you can use the pamphlet when you get home to continue to process this information. Just know your medications and why you’re taking them.”
Advertisement
This article originally appeared in Cleveland Clinic Men’s Health Advisor.
Advertisement

Delivered every Tuesday!
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more
It's a letter about the news!

Every two weeks once
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
Certain seizure medications, HIV treatments, antibiotics or herbal supplements can make your oral contraception less effective
Some types of expired meds may not be harmful, but they probably aren’t worth the risk
Options for sober social drinking are abundant, but be mindful about additives and triggers
‘Rebound congestion’ happens when your body starts to rely on decongestant nasal spray
This diabetes med can treat obesity, but it’s not for people who just want to drop a few pounds
Learn how a little quiet time can make a big difference
Cutting pills is a normal — and potentially dangerous — practice
If you’re not sure, talk to your healthcare provider — first
Type 2 diabetes isn’t inevitable with these dietary changes
Applying a hot or cold compress can help with pain
Pump up your iron intake with foods like tuna, tofu and turkey