Formerly used as a treatment, they’re not as effective against current strains of COVID-19
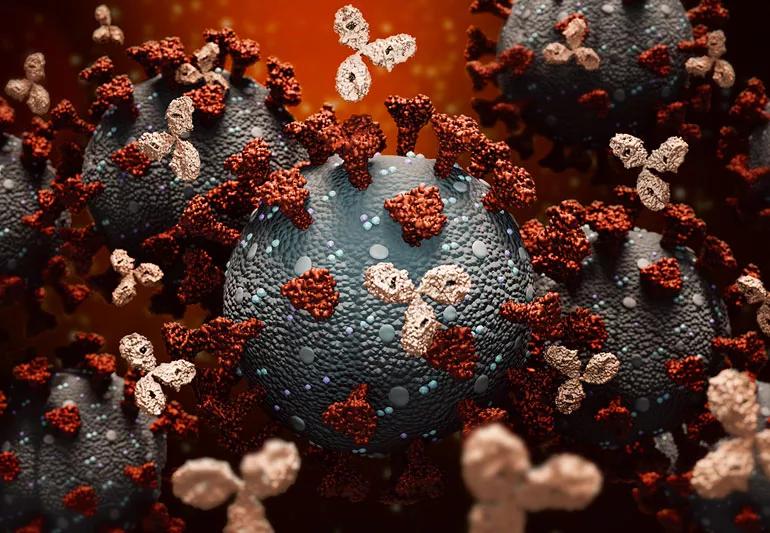
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5a5101b6-fbca-4612-9f1f-20edd693a4e9/MonoclonalAntibodiesCovid-1218792909-770x533-1_jpg)
Monoclonal Antibodies attacking coronavirus
Our immune system is a pretty powerful tool capable of fighting off everyday infections. But sometimes, when faced with more severe illnesses like cancer, our immune system could use an additional boost. One such boost comes in the form of lab-made monoclonal antibodies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Infections disease specialist Tricia Bravo, MD, breaks down this very scientific-sounding term and explains how monoclonal antibodies were used earlier in the pandemic to prevent severe COVID-19 infections in people who were at higher risk for serious illness.
When you’re exposed to an infection, your body makes specific proteins called antibodies that are designed to fight off that infection. When you no longer have that infection, your body continues to produce some of those antibodies in case the infection returns.
“Antibodies are basically proteins that your body makes to fight a specific infection,” explains Dr. Bravo.
Monoclonal antibodies are lab-made antibodies that mimic what your natural antibodies are able to do, but they tend to work faster with more immediate results. Monoclonal antibodies are most often used as a form of targeted therapy for specific kinds of cancer, but they’ve also been used throughout the pandemic to help fight off COVID-19.
“It’s very specific ammunition to fight particular infectious organisms,” Dr. Bravo adds.
Neutralizing monoclonal antibodies are no longer used to treat COVID-19 in the U.S. because they’re not as effective against currently circulating omicron subvariants.
Advertisement
Currently in the U.S., the main treatment options that target COVID-19 directly are these antiviral medications:
These are available for people with mild to moderate COVID-19 infection who are at high risk for progressing to severe infection. Remdesivir is also a recommended treatment strategy in conjunction with steroids for certain people who are hospitalized with severe illness.
Earlier in the pandemic, monoclonal antibodies like Evusheld™ (tixagevimab and cilgavimab) were once used as a preventive measure against COVID-19. These neutralizing monoclonal antibodies have a different mechanism of action from antivirals.
“That means neutralizing monoclonal antibodies work differently from antiviral medications by attaching to the spike protein on the surface of the COVID-19 virus and preventing it from infecting your cells,” explains Dr. Bravo. “Antiviral medications, on the other hand, stop the virus from making copies of itself and reduces the spread of infection.”
Now, the U.S. Food and Drug Administration (FDA) has withdrawn emergency use authorization for monoclonal antibodies that have been previously used as treatment.
The monoclonal antibodies that are no longer authorized in the U.S. (but may be authorized in other areas outside of the U.S.) include:
Other monoclonal antibodies, like Actemra® (tocilizumab), are only used as treatment in the U.S. for people who are hospitalized with severe COVID-19 infection who meet the following criteria:
This medication doesn’t target the coronavirus directly, but it’s an anti-inflammatory that stops your immune system from becoming overreactive to the virus. This medication has also been used to treat other inflammatory conditions like rheumatoid arthritis.
The recommendations for COVID-19 treatments and the use of monoclonal antibodies changes often to meet the demand of up-and-coming variants. For the most up-to-date information, the FDA offers a list of treatments that have been given emergency use authorization (EUA) for treating COVID-19. The National Institutes of Health (NIH) continues to update its guidelines with new effective treatments, alongside a list of old treatments that have become ineffective. And for people outside of the U.S., the World Health Organization (WHO) offers its own set of guidelines on which treatments are recommended.
Advertisement
Monoclonal antibodies are only given through an IV or as a subcutaneous injection (a shot). That means, in order to receive them, you need to be seen in a medical setting, which limits the overall availability of the treatment.
When used as a treatment for COVID-19, Actemra is given through a single 60-minute IV infusion.
Don’t think of monoclonal antibodies as an alternative to the COVID-19 vaccine. Dr. Bravo stresses that getting vaccinated is still your body’s single best protection against contracting severe COVID-19. That’s true even if you’re immunocompromised.
“I can’t emphasize enough the importance of vaccines,” she says. “They offer a much better kind of protection and a much more lasting protection than you can get with monoclonal antibodies.”
Advertisement

Delivered every Tuesday!
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more
It's a letter about the news!

Every two weeks once
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
The short answer: It’s complicated, but the basic care precautions still prevail, like washing your hands and isolating if you’re sick
They can feel like a typical headache or a migraine headache, but the pain can last for weeks to months
Any large social gathering — from a family birthday party to an indoor music concert — has the potential to spread serious infection
It’s important to connect with a healthcare provider, get quality sleep and balance your activities with your energy levels
Symptoms can overlap and be hard to distinguish, but there are some telltale differences
Just like the flu, COVID-19 will continue to evolve every year
It’s best to treat flu-like symptoms as if you have COVID-19
The duration varies, but symptoms can linger for a few days up to a couple weeks or more
Type 2 diabetes isn’t inevitable with these dietary changes
Applying a hot or cold compress can help with pain
Pump up your iron intake with foods like tuna, tofu and turkey