How the coronavirus causes acute respiratory distress syndrome
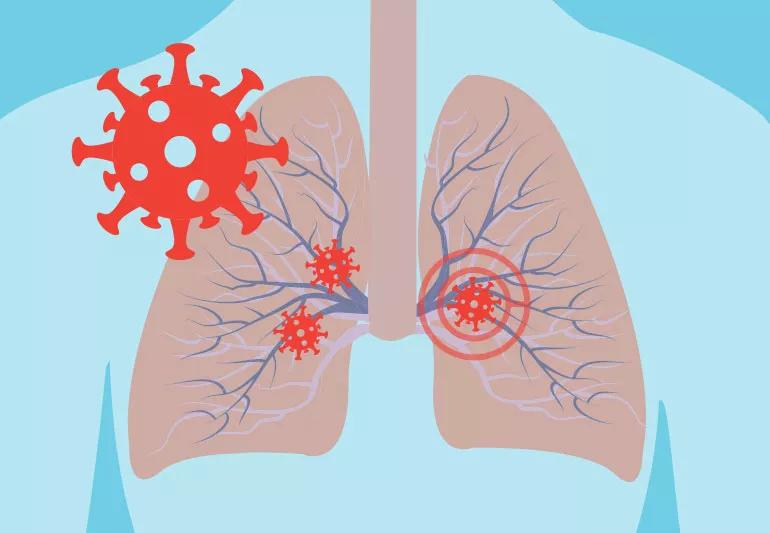
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0cfd969a-08af-4b78-895e-af5ba6bcb760/caronavirusLungs-125957837-770x533-1_jpg)
coronavirus and the lungs
As the coronavirus (COVID-19) outbreak continues, we’re learning more about the disease, what it does to the body and the damage it can cause. But not sure you understand yet exactly what the virus can do to you?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Although many people with COVID-19 have no symptoms or only mild symptoms, a subset of patients develop severe respiratory illness and may need to be admitted for intensive care.
In a new video, lung pathologist Sanjay Mukhopadhyay, MD, lays out in detail how the lungs are affected in these severe cases. The 15-minute video walks through how COVID-19 causes a “dangerous and potentially fatal” condition known as acute respiratory distress syndrome (ARDS) while providing stark images that underscore the severity of the damage that condition can cause to your lungs.
As Dr. Mukhopadhyay explains, Chinese researchers have linked COVID-19 to ARDS. Their study examined risk factors for 191 confirmed coronavirus patients who died while being treated in two hospitals in Wuhan, China.
The researchers found 50 of the 54 patients who died had developed ARDS while only nine of the 137 survivors had ARDS.
“It’s a really, really significant contribution to death in these patients,” says Dr. Mukhopadhyay.
If you have ARDS, you’ll have symptoms like sudden breathlessness, rapid breathing, dizziness, rapid heart rate and excessive sweating.
But the four main things doctors will look for are:
Advertisement
Most importantly, patients who are suffering from ARDS end up having damage to the walls of the air sacs in their lungs — the ones that help oxygen pass through into our red blood cells. That’s what doctors term diffuse alvelolar damage.
In a healthy lung, oxygen within these air sacs (alveolus) travels through to small blood vessels (capillaries). These tiny vessels, in turn, deliver the oxygen to your red blood cells.
“Nature has evolved in a way that the wall of alveolus is very, very thin in a normal person so oxygen can easily get from the air space in between to the red blood cell,” Dr. Mukhopadhyay explains.
The coronavirus damages both the wall and lining cells of the alveolus as well as the capillaries. The debris that accumulates because of all of that damage lines the wall of the alveolus the same way paint would cover a wall, Dr. Mukhopadhyay points out. The damage to capillaries also causes them to leak plasma proteins that add to the wall’s thickness.
“Eventually, the wall of the alveolus gets thicker than it should be,” he notes. “The thicker this wall gets, the harder it is to transfer oxygen, the more you feel short of breath, and the more and more you start moving towards severe illness and possibly death.”
The whole point, Dr. Mukhopadhyay stresses, is to emphasize what the coronavirus is capable of doing to a body, particularly high-risk patients who may be more vulnerable to infection. He hopes this will get people to take the current outbreak seriously.
“Please don’t dismiss this as ‘just another viral infection that will pass,'” he says. “Please take all the precautions that the CDC is outlining. Please protect yourself, your family, and others.”
Advertisement

Delivered every Tuesday!
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more
It's a letter about the news!

Every two weeks once
Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
The short answer: It’s complicated, but the basic care precautions still prevail, like washing your hands and isolating if you’re sick
They can feel like a typical headache or a migraine headache, but the pain can last for weeks to months
Any large social gathering — from a family birthday party to an indoor music concert — has the potential to spread serious infection
It’s important to connect with a healthcare provider, get quality sleep and balance your activities with your energy levels
Just like the flu, COVID-19 will continue to evolve every year
The duration varies, but symptoms can linger for a few days up to a couple weeks or more
Vaccination is best for prevention, but if you get sick with COVID-19, treatments are available
The virus lives best in humans, but it can last on hard surfaces, like doorknobs and railings
Type 2 diabetes isn’t inevitable with these dietary changes
Applying a hot or cold compress can help with pain
Pump up your iron intake with foods like tuna, tofu and turkey