FDA-approved nerve stimulator helps open your airway
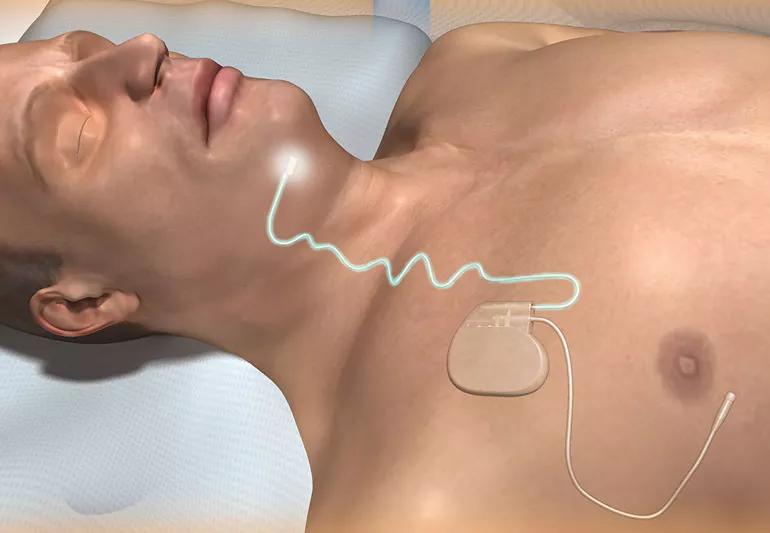
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1f385736-0d42-4352-81d7-0de1cdf2ae8b/CPAPoption-1409-IM-photo1-770x533_jpg)
Implantible device replacement for CPAP
If you have obstructive sleep apnea, your airway tends to collapse when you sleep. After snoring, gasping and choking your way through the night, you’re getting by on little rest the next day.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The most common solution is CPAP (continuous positive airway pressure). While your partner may appreciate quieter nights, chances are you’re not a big fan.
“It’s the standard treatment for obstructive sleep apnea, but about half the people don’t like it very much,” explains surgical sleep medicine specialist Alan Kominsky, MD.
A Cleveland Clinic study found that just 44% of the patients prescribed CPAP for obstructive sleep apnea were still using it three years later.
That means a significant number of patients are not being treated for obstructive sleep apnea, which can lead to hypertension, stroke and cardiac problems.
Dental appliances can help patients with mild to moderate obstructive sleep apnea. Surgery to remove obstructive tissue is also an option. But it’s invasive and requires an extensive recovery.
Another option is an implantable, programmable device approved by the U.S. Food and Drug Administration in 2014. The Inspire® upper airway stimulation device looks like a heart pacemaker.
It has two leads. One senses your breathing. The other stimulates the nerve that controls the tongue, to move it forward and open your throat.
“A pivotal trial demonstrated the device’s safety and effectiveness in a small group of patients with moderate to severe obstructive sleep apnea,” says Dr. Kominsky. Five years later, those improvements have been measured and are persistent.
Advertisement
The airway stimulation device is available at select U.S. medical centers, including Cleveland Clinic. To be eligible for it:
Eligible patients must have a recent sleep study. The next step is to perform sleep endoscopy. This outpatient procedure begins with sedation so that doctors can insert an endoscope into the airway. This lets them view the pattern of airway collapse to confirm the device will help.
The stimulator system is then implanted under general anesthesia in an outpatient procedure.
“One month after the procedure, we turn the device on,” says Dr. Kominsky. “One month after that, we perform a repeat sleep study. This helps us make adjustments to ensure the device will deliver the maximum benefit.”
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
Ignoring the warning signs could put you at risk for serious health issues
Sleeping disorder may increase danger of cardiac event
Learn which type of sleep test is right for you
New study points out need for increased awareness
Mouth taping isn’t a recommended treatment for sleep apnea or snoring
Here’s what to know from a sleep medicine specialist
This connection is yet another reason to seek help for OSA
The short answer from a cardiovascular researcher
Type 2 diabetes isn’t inevitable with these dietary changes
Applying a hot or cold compress can help with pain
Pump up your iron intake with foods like tuna, tofu and turkey